People
My group brings together a talented and dedicated group of passionate students and researchers who bring together a combination of expertise in islet biology, electrophysiology, microscopy, gene editing, and computational biology. Together we unravel how pancreatic islets work, in order to devise therapeutic strategies to fix them when they break down in diabetes.
Dr. Mark O. Huising

Contact: mhuising@ucdavis.edu
Dr. Talitha van der Meulen
 Talitha received her PhD in developmental biology studying muscle development in zebrafish at Wageningen University in the Netherlands. After studying biochemistry at San Diego State University and diabetes at the Salk Institute in La Jolla she helped set up the Huising diabetes research lab at UC Davis. These days she is an assistant professor of teaching at UC Davis, teaching NPB110A, NPB10 and NPB101L. She is leading a team of professors to enhance equity and inclusion in the NPB curriculum by updating the program learning outcomes (what students should be able to do when they graduate with an NPB degree) and implementing assessment strategies to actually find out if these program learning outcomes are met. After 2 years of Covid-19-related cancellations, her study abroad program for NPB110A in the Netherlands looks like it will be taking off in Summer 2022. She is still associated with the Huising lab and joins in lab meetings, but cannot spend much time there because of teaching. In her spare time, Talitha enjoys her family, cat, baking, camping, hiking and exploring California and nearby states.
Talitha received her PhD in developmental biology studying muscle development in zebrafish at Wageningen University in the Netherlands. After studying biochemistry at San Diego State University and diabetes at the Salk Institute in La Jolla she helped set up the Huising diabetes research lab at UC Davis. These days she is an assistant professor of teaching at UC Davis, teaching NPB110A, NPB10 and NPB101L. She is leading a team of professors to enhance equity and inclusion in the NPB curriculum by updating the program learning outcomes (what students should be able to do when they graduate with an NPB degree) and implementing assessment strategies to actually find out if these program learning outcomes are met. After 2 years of Covid-19-related cancellations, her study abroad program for NPB110A in the Netherlands looks like it will be taking off in Summer 2022. She is still associated with the Huising lab and joins in lab meetings, but cannot spend much time there because of teaching. In her spare time, Talitha enjoys her family, cat, baking, camping, hiking and exploring California and nearby states.
Graduate Students
Michelle Chan
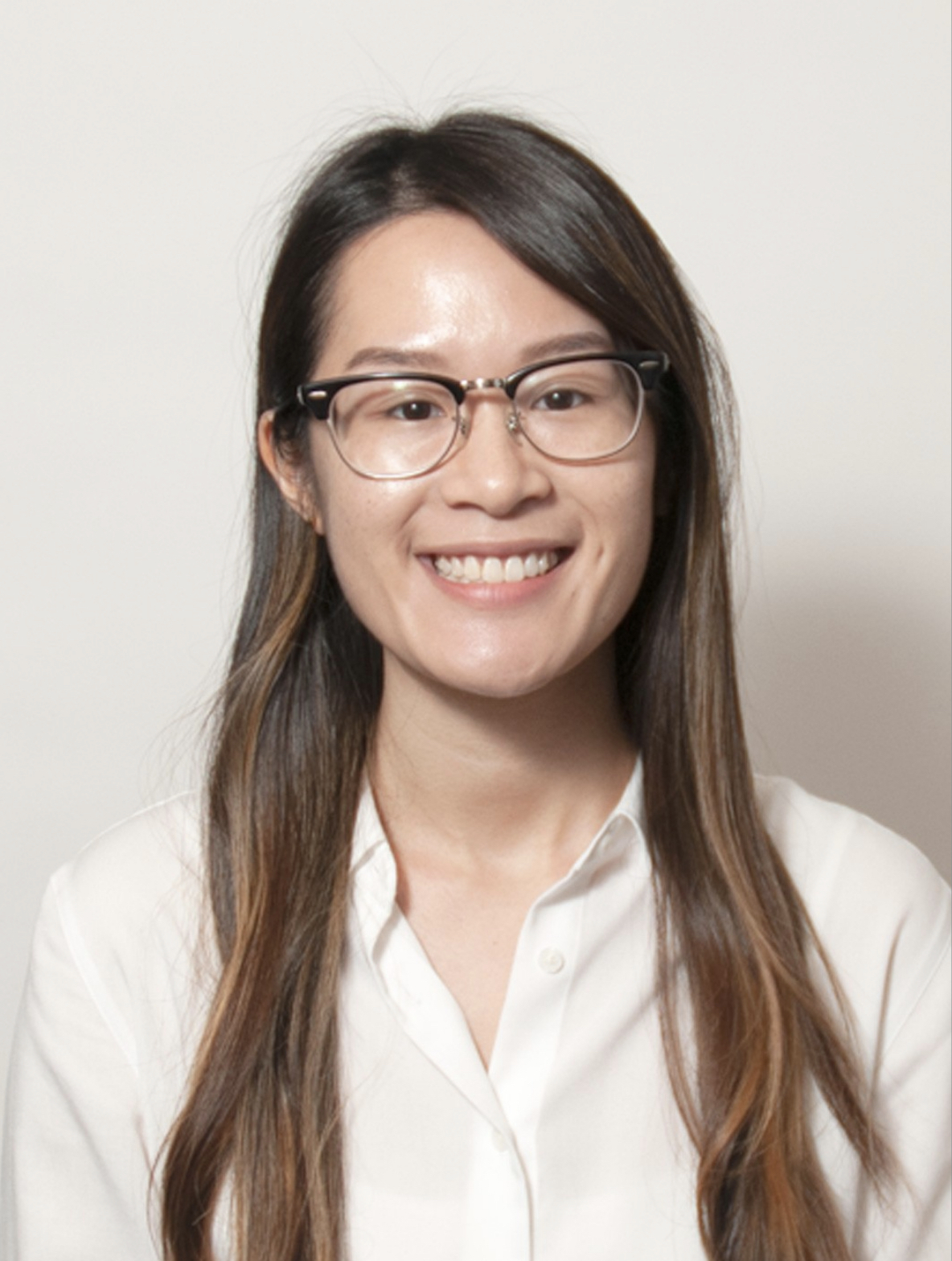 Michelle is a graduate student in the BMCDB PhD program at UC Davis. She graduated with a BS in Biochemistry and Cell Biology from UC San Diego, where she had the opportunity to conduct research in labs at the Salk Institute for Biological Studies, Scripps Research, and UC San Diego School of Medicine. After graduation, she worked in the lab of Dr. Steve Finkbeiner at the Gladstone Institutes to investigate the molecular mechanisms of amyotrophic lateral sclerosis. Michelle’s interest in investigating cell signaling drew her to the Huising lab for her doctoral work, and she is excited to learn more about islet biology. Aside from research, she likes to read, visit new coffee shops, and watch Netflix in her free time.
Michelle is a graduate student in the BMCDB PhD program at UC Davis. She graduated with a BS in Biochemistry and Cell Biology from UC San Diego, where she had the opportunity to conduct research in labs at the Salk Institute for Biological Studies, Scripps Research, and UC San Diego School of Medicine. After graduation, she worked in the lab of Dr. Steve Finkbeiner at the Gladstone Institutes to investigate the molecular mechanisms of amyotrophic lateral sclerosis. Michelle’s interest in investigating cell signaling drew her to the Huising lab for her doctoral work, and she is excited to learn more about islet biology. Aside from research, she likes to read, visit new coffee shops, and watch Netflix in her free time.
Ryan Hart
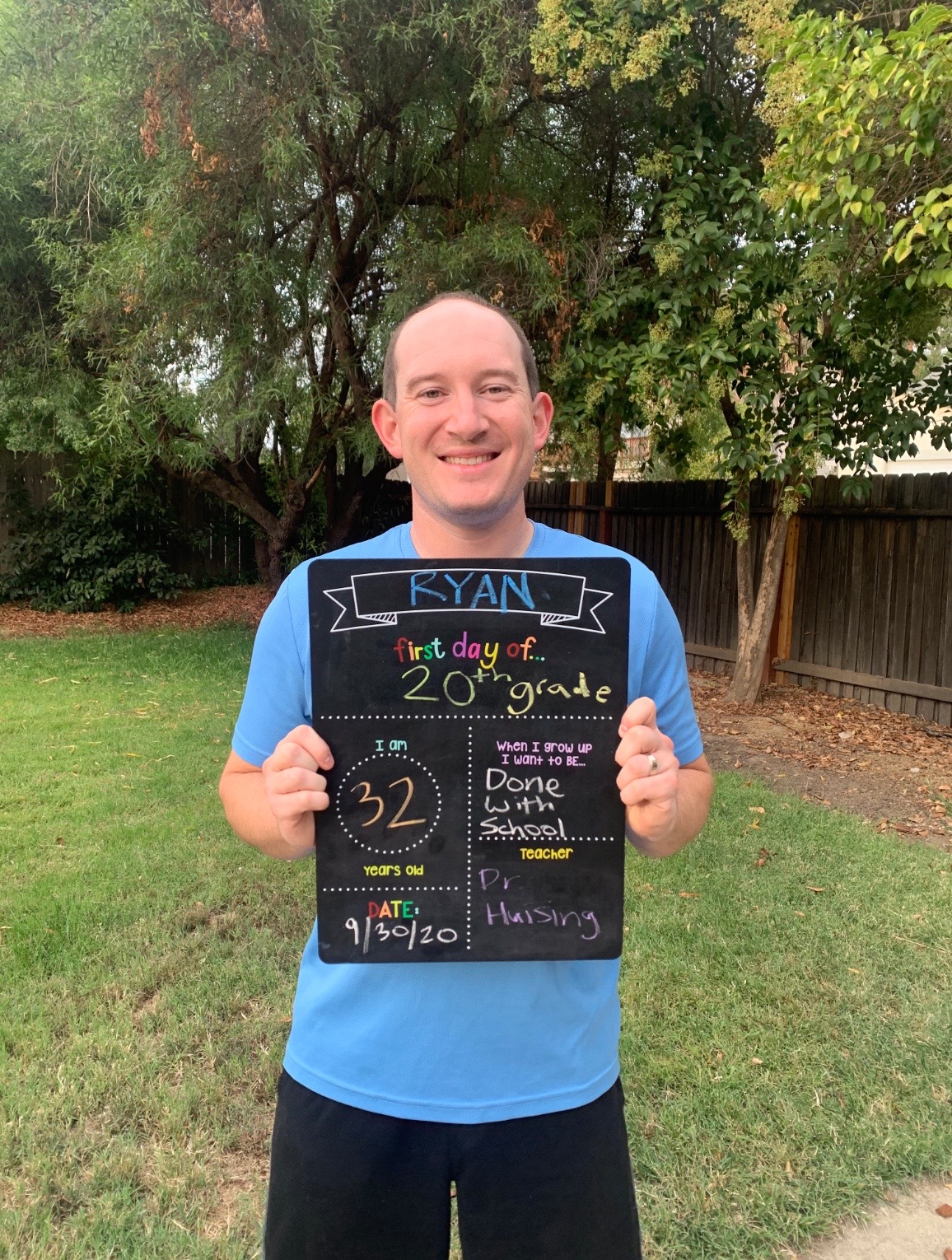 Ryan is a graduate student in the Biochemistry, Molecular, Cellular & Developmental Biology (BMCDB) Ph.D. program at UC Davis. He graduated from Truman State University in 2011 with a B.S. in Biology, and A.T. Still University in 2013 with an M.S. in Biomedical Science. Prior to joining the Huising Lab, he studied actomyosin associated cytoskeletal forces in the lab of Dr. Indra Chandrasekar at the University of South Dakota. In his free time he enjoys exploring California with his wife Kimmy, his daughter Allie, and their dog Jethro.
Ryan is a graduate student in the Biochemistry, Molecular, Cellular & Developmental Biology (BMCDB) Ph.D. program at UC Davis. He graduated from Truman State University in 2011 with a B.S. in Biology, and A.T. Still University in 2013 with an M.S. in Biomedical Science. Prior to joining the Huising Lab, he studied actomyosin associated cytoskeletal forces in the lab of Dr. Indra Chandrasekar at the University of South Dakota. In his free time he enjoys exploring California with his wife Kimmy, his daughter Allie, and their dog Jethro.
Mohammad Pourhosseinzadeh
 Mohammad graduated from UC Davis with a B.S. in Biochemistry and Molecular Biology and is a current MD/PhD student. While a student at UC Davis, he gained an interest in research studying meiotic recombination in yeast. His interest in research and its applications in medicine drove him to join the Huising lab. In his free time he enjoys watching Netflix and reading.
Mohammad graduated from UC Davis with a B.S. in Biochemistry and Molecular Biology and is a current MD/PhD student. While a student at UC Davis, he gained an interest in research studying meiotic recombination in yeast. His interest in research and its applications in medicine drove him to join the Huising lab. In his free time he enjoys watching Netflix and reading.
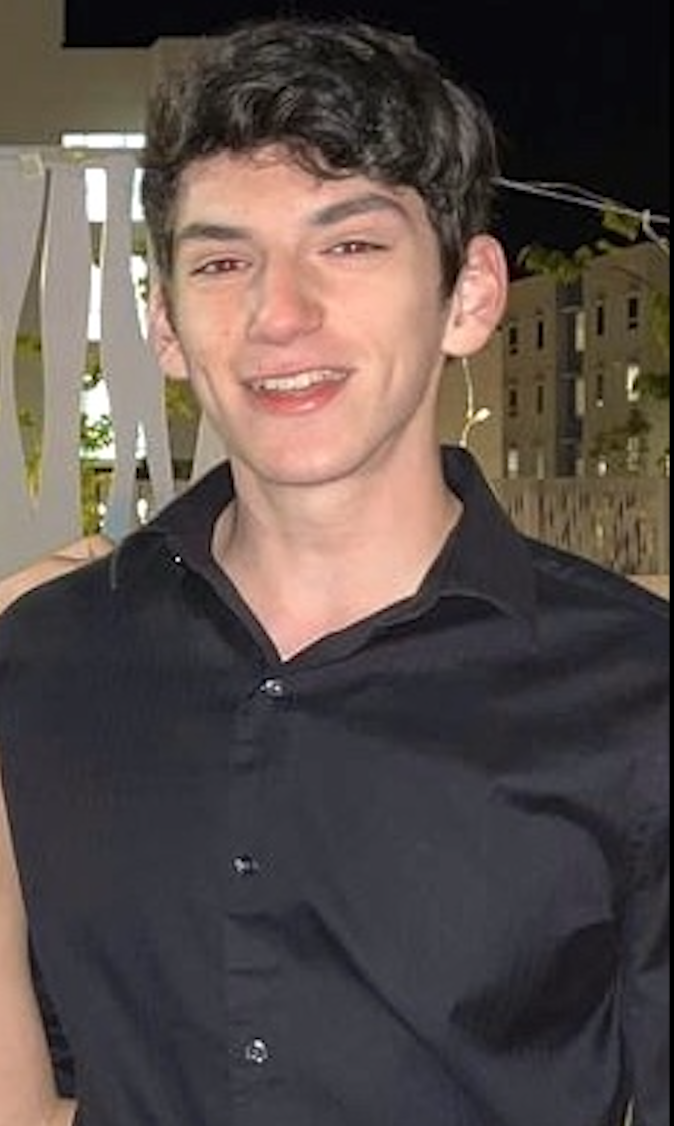
Max Shin
Nathan Cook
 Nathan is graduate student in the BMCDB PhD program at UC Davis. He graduated with a BS in bimolecular engineering from UC Santa Cruz, where he had the opportunity to study MAPK signaling's regulation of Nanog in mouse embryonic stem cells under Ali Shariati. The Huising Lab's research caught his eyes as an interesting intersection of his interest in cellular regulation and differentiation from his undergrad research and his long standing interest in beta cell biology and diabetes. His research now focuses on the functional heterogeneity mouse beta cells display, and differences in calcium behavior between different beta cell model systems. In his free time Nathan enjoys reading, fencing, and playing board games, especially with friends.
Nathan is graduate student in the BMCDB PhD program at UC Davis. He graduated with a BS in bimolecular engineering from UC Santa Cruz, where he had the opportunity to study MAPK signaling's regulation of Nanog in mouse embryonic stem cells under Ali Shariati. The Huising Lab's research caught his eyes as an interesting intersection of his interest in cellular regulation and differentiation from his undergrad research and his long standing interest in beta cell biology and diabetes. His research now focuses on the functional heterogeneity mouse beta cells display, and differences in calcium behavior between different beta cell model systems. In his free time Nathan enjoys reading, fencing, and playing board games, especially with friends.
Catherine Dombroski
 Catherine is a DVM/PhD student in the Molecular, Cellular and Integrative Physiology (MCIP) program at UC Davis. She graduated with a BS in Biochemistry and minor in Biomedical Research from UCLA where she had the opportunity to conduct research in Dr. Karen Reue's lab investigating the role of genetics on sex differences in obesity. She has always had an interest in the underlying mechanisms driving metabolic disease, which drove her to join the Huising lab where she could utilize her veterinary background to further understand islet biology. In her free time, she enjoys hiking, gardening, and attending concerts.
Catherine is a DVM/PhD student in the Molecular, Cellular and Integrative Physiology (MCIP) program at UC Davis. She graduated with a BS in Biochemistry and minor in Biomedical Research from UCLA where she had the opportunity to conduct research in Dr. Karen Reue's lab investigating the role of genetics on sex differences in obesity. She has always had an interest in the underlying mechanisms driving metabolic disease, which drove her to join the Huising lab where she could utilize her veterinary background to further understand islet biology. In her free time, she enjoys hiking, gardening, and attending concerts.
Junior Specialist - Lab Manager
Naomi Cinque

Jordan Lee

Rashita Chauhan

Undergraduate Researchers
Jordan Lee

Anishka Mangrulkar

Sriansh Pasumarthi

Joel Sanchez
Taven Cunningham

Ramir Tirado

Karen Zhai

Pierre Napaa

Harnejan Atwal

Abby Gailmard

Jacob Boi

Seth Kim

Sharlene Lee

Muskaan Wadhava
